Author: Manuel J. Arroyo Pulgar
Health care-associated infections (HAIs) occur when receiving health care for another condition [1]. These infections can happen in any health-care facility and can be caused by any pathogen. A bigger problem in these HAIs is when the pathogen that caused the infection has an antibiotic resistance, something we talked about in our previous post. In fact, these drug-resistant diseases could cause 10 million deaths each year by 2050 along with a huge economic burden [2].
One group of these drug-resistant pathogens is known by the name ESKAPE, an acronym composed by their names and a clear reference to their ability to escape the effects of commonly used antibiotics through different mechanisms like post-translational modifications:
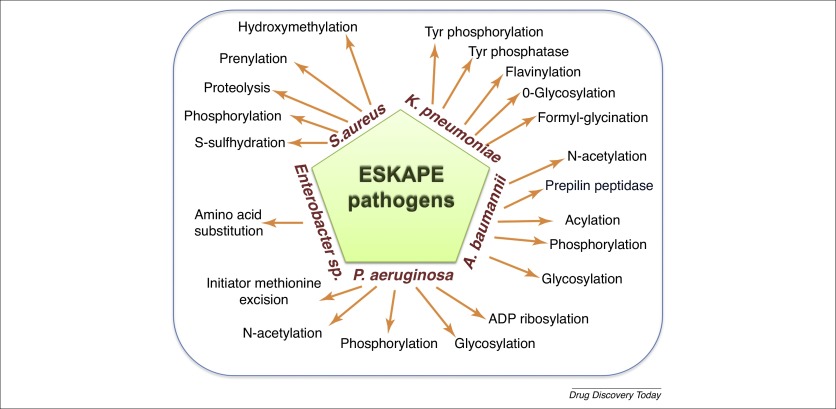
These pathogens are:
- Enterobacter sp.
- Staphylococcus aureus
- Klebsiella pneumoniae
- Acinetobacter baumanii
- Pseudomonas aeruginosa
- Enterococcus faecium
A few of these bacteria are mentioned even for the 2019 CDC Report like the Acinetobacter sp. which caused 8500 hospitalizations and 700 deaths in 2017 in US. Staphylococcus aureus is commonly found as part of the human skin microbiota but can cause infections in ectopic places like wounds. In the case of Pseudomonas aeruginosa infections usually occur in people with weakened immune systems and can be particularly dangerous for patients with chronic lung diseases. Some strains of Enterobacter sp. can cause blood and urinary tract infections and there are only two effective antibiotics (Tigecycline and Colistin) versus these resistant strains. There are even some K. pneumoniae carbapenem-resistant (CRKP) besides that certain of these strains have also developed beta-lactamases. Enterococci group can cause serious infections for patients in health-care settings, including bloodstream, surgical site and urinary tract infections just like Enterobacter sp.. In the case of E. faecium, the estimated cases in hospitalized patients in 2017 and deaths was 54500 and 5400 respectively.

In Clover Biosoft, we believe that the mass spectrometry technology and the processing of its data can help to improve the diagnosis (in time and cost) of these infections with the purpose of reducing the time and all the complications associated to these multi-drugs resistant bacteria. That’s why Clover Biosoft is collaborating closely with hospitals that have this emergent problem in their facilities and patients. In fact, data of the ESKAPE pathogens spectra are well-known to us.
REFERENCES:
[1] https://health.gov/hcq/prevent-hai.asp
[3] https://www.sciencedirect.com/science/article/pii/S1359644618302873
